More ambitious IBD treatment targets are within reach
Recent years have seen an emergence of potential new treatment options in IBD, allowing for more ambitious targets and treatment goals[1][2]
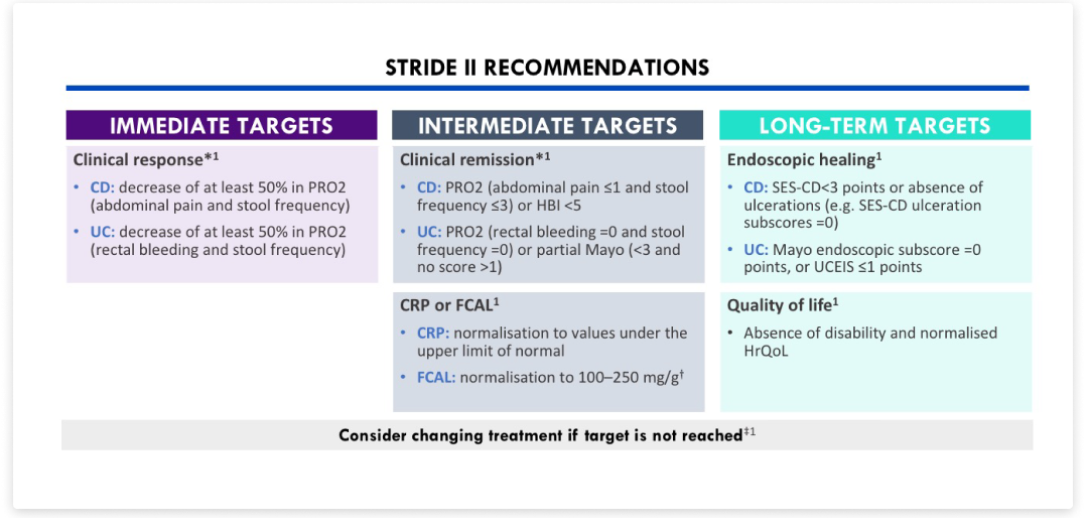
STRIDE II recommendations[1]
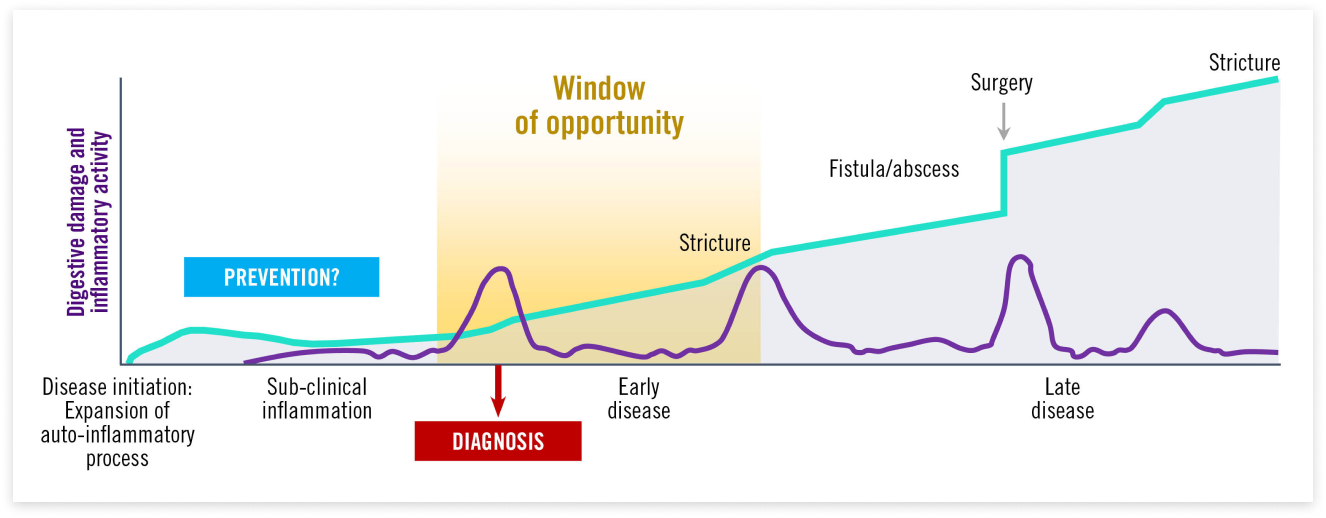
Early intervention is key in defining the right path for long-term remission[3][4][5][6][7]
IBD, which includes CD and UC, is a chronic progressive disease that without adequate and timely treatment could lead to irreversible damage.[3][4]
Early effective treatment during the window of opportunity with disease-modifying agents could prevent disease progression[5]
The first advanced therapy is critical in IBD to determine long-term patient outcomes[3][4][5][6][7][8][9]
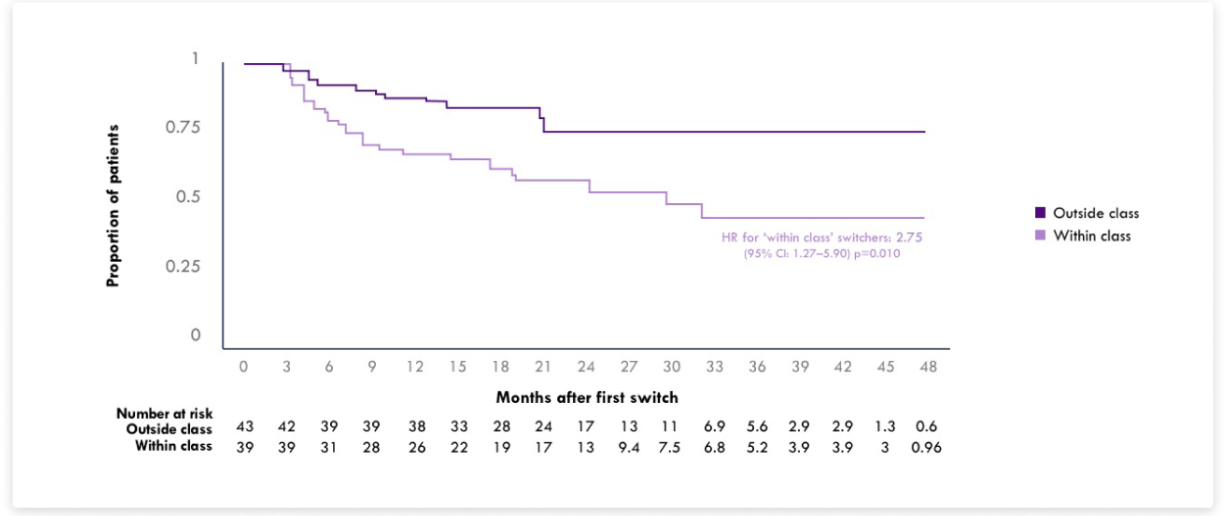
Switching to a different biologic may increase treatment persistence vs anti-TNFα cycling[8]
In patients with CD experiencing loss of response with adalimumab or infliximab, switching to a treatment with a different MoA resulted in higher probability of persisting with subsequent treatment than for those who switched to a different anti-TNFα.[8]
MITRORS study: time to treatment re-switch to another biologic§[8]
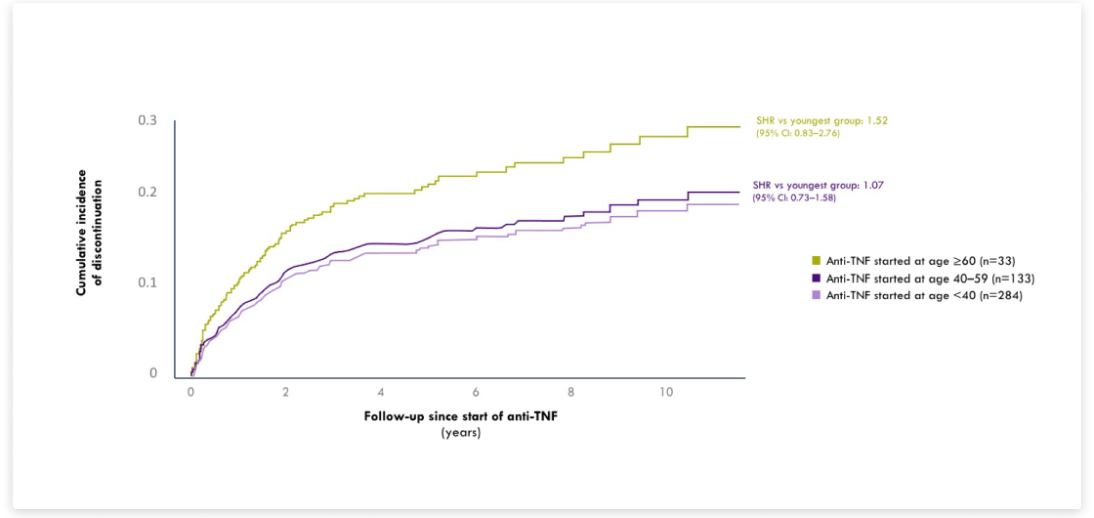
Older age has been associated with a higher incidence of AEs and serious infections during anti-TNF treatment[9]
In elderly patients (aged ≥60 years) with IBD, initiating anti-TNF therapy resulted in higher discontinuation rates due to AEs than for younger patients.[9]
IBDREAM registry: cumulative incidence of treatment discontinuation due to AEs in patients initiating anti-TNF therapy by age group[9]
Discover how we support ambitious treatment goals
* Clinical response or remission are insufficient to be used as long-term targets.[1]
† The cutoff value of faecal calprotectin is dependent on the desired outcome. Lower thresholds (e.g., <100 mg/g) have been proposed for reflecting deep healing (both endoscopic and transmural healing) or histological healing, whereas higher values (e.g., <250 mg/g) reflect less stringent outcomes (e.g., MES of 0 or 1 in UC).[1]
‡ Time to reach clinical response varies based on therapy and mechanism of action.[1]
§ Patients were classified as either within-class switchers if they switched to adalimumab or infliximab, or outside-class switchers if they switched to vedolizumab or ustekinumab.[8]
AE: Adverse event; CD: Crohn’s disease; CI: Confidence interval; CRP: C-reactive protein; FCAL: Faecal calprotectin; HBI: Harvey-Bradshaw Index;
HR: Hazard ratio; HrQoL: Health-related quality of life; MoA: mode of action; PRO: Patient-reported outcome; SES-CD: Simple endoscopic score in CD;
SHR: Subhazard rate; STRIDE: Selecting Therapeutic Targets in Inflammatory Bowel Disease; TNF: Tumour necrosis factor; UC: Ulcerative colitis;
UCEIS: Ulcerative colitis endoscopic index of severity.