Molecular subtypes of advanced UC

How understanding molecular subtypes of advanced UC could impact management approaches
A far more detailed understanding of advanced urothelial carcinoma (UC) has resulted in the identification of distinct molecular subtypes.[1] Understanding the molecular subtypes of UC can help to identify distinct patient populations and improve treatment decision-making.[1][2]
Listen to Dr. Ignacio Durán, Medical Oncologist at Hospital Universitario Marqués de Valdecilla in Santander, talking about why he believes we are moving towards a biomarker-led approach to care in advanced UC.
Find out what the consensus classification of muscle invasive bladder cancer subtypes could mean for how we view advanced UC and what it means for the role of molecular pathology.[1][2]
The current approach to advanced UC
.png?width=1284&height=608&format=png&quality=50)
A bladder cancer patient’s chance of survival is highly stage dependent and progression from muscle invasive bladder cancer (MIBC) to metastasis is common:[3][4][5]
- Despite guideline-recommended radical cystectomy, approximately 50% of patients with MIBC will relapse[6]
- Local recurrence accounts for 30% of relapses, whereas distant metastases are more common[6]
The treatment approach in mUC remains controversial, where evidence in some areas of bladder cancer management is limited and/or conflicting.[7]
Furthermore, the efficacy of immunotherapies and antibody-drug conjugates in FGFR+ patients has not been studied.[8][9]
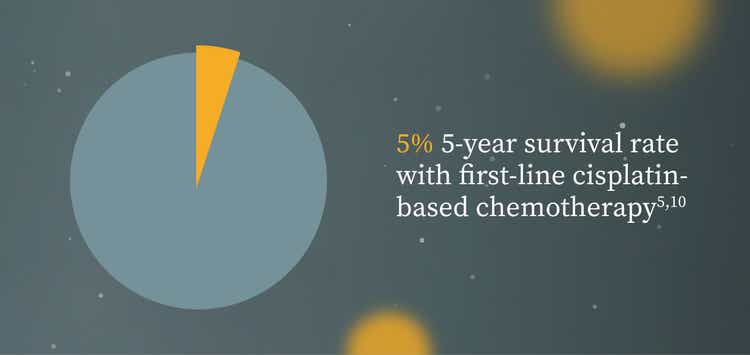
- For over 30 years, the standard first-line treatment option has been broad-acting cisplatin-based chemotherapy, with a 5-year survival rate as low as 5%[5][10]
- The use of biomarkers in the management of mUC is low,[11][12][13] and second-line treatment options are limited to conventional chemotherapy agents or programmed death protein/ligand 1 inhibitors, which have response rates of 10-21%[6][14][15][16][17]

Molecular subtypes of advanced UC
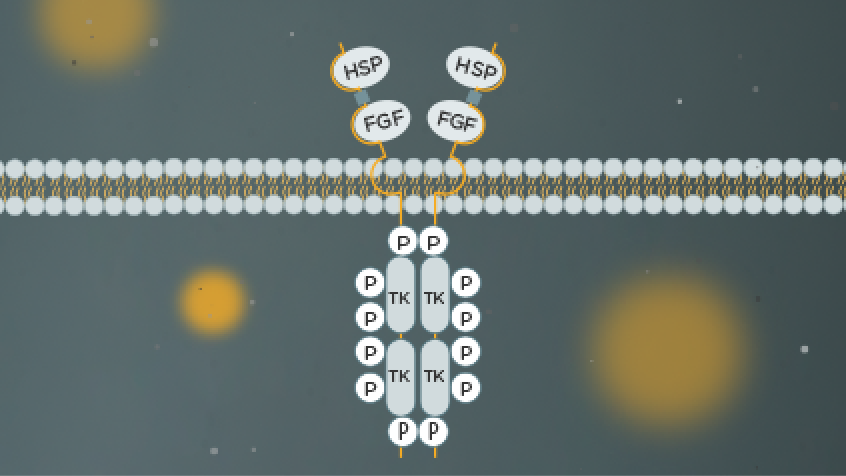
The molecular biomarkers and pathways involved in UC are key to understanding its biological heterogeneity and identifying specific subtypes that may be used to predict clinical outcomes and treatment responsiveness[2]
- Molecular subtypes of MIBC have been associated with different responses to treatments such as chemotherapy or immunotherapy[1][19][20]
The molecular understanding of MIBC has led to a consensus classification of tumour classes with distinct oncogenic mechanisms[1]
- In a recent international consensus, a six-class molecular classification system of MIBC was established[1]
- 1750 tumour samples were studied[1]
- Each molecular subtype of MIBC has distinct:[1]
- Differentiation patterns
- Oncogenic mechanisms
- Tumour microenvironments
- Histological characteristics
- Clinical associations
- Luminal papillary (24%) and basal/squamous (35%) are the two most common classes of MIBC (Figure 1)[1]
- Other classifications include neuroendocrine-like (3%), luminal nonspecified (8%), luminal unstable (15%), and stroma-rich (15%)[1]
Figure 1. Six-class molecular classification system of MIBC
Adapted from Kamoun A et al. 2020.[1]
Figure legend can be found in footnotes at the bottom of the page.
In other cancer types, improved understanding of molecular pathology has enabled biomarker-led precision medicine that can improve outcomes for appropriately selected subsets of patients[21][22]
The identification of targets in tumours such as colorectal, breast, ovarian and non-small cell lung cancer has led to the development of targeted therapies[22]
Targeting tumours with inhibitors that block aberrant signalling has improved patient outcomes across different cancers, providing efficacy and toxicity benefits[21][22]
Fibroblast growth factor receptor (FGFR) alterations in UC
FGFR alterations are more prevalent in UC than in any other human cancer[23]
The type of FGFR alterations most commonly found can differ in different cancer types, with FGFR3 mutations predominating in bladder and other urothelial tumours.[23]
The incidence of FGFR alterations in 126 UC cases was established by Helsten T et al. (Figure 2), with the dataset representing urothelial (transitional cell) cancer of the bladder, renal pelvis, and ureter.[23] This dataset did not include cases of bladder sarcoma, small cell carcinoma, squamous cell carcinoma, or neuroendocrine carcinoma.[23]
Figure 2. Incidence of FGFR alterations in 126 UC cases
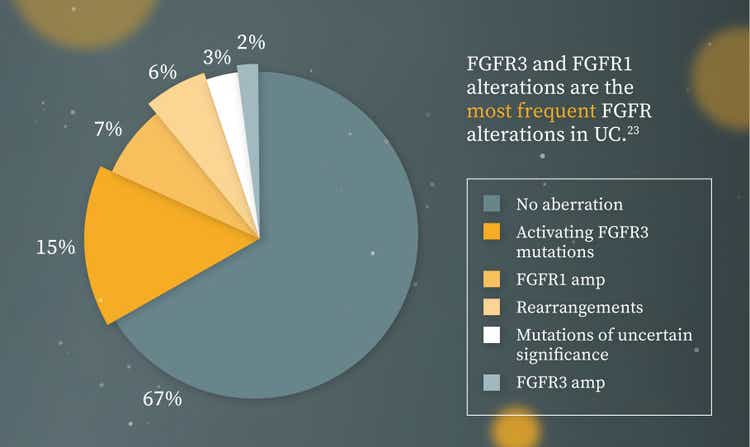
Adapted from Helsten T et al. 2016.[23]
Figure legend can be found in footnotes at the bottom of the page.
Up to one in five of your advanced UC patients may have FGFR alterations[24]

FGFR alterations are found in both advanced and non-muscle invasive bladder cancer (NMIBC) stages.[5][24][25]
- FGFR3 alterations have been found in up to 80% of Ta NMIBC tumours[5]
- A study of 52 advanced UC patients found a total of 10 patients (19.2%) had FGFR alterations (9 mutations of FGFR3 and 1 FGFR2:CASP7 translocation)[24]
Figure 3. Presence of FGFR3 mutations by tumour stage

Adapted from Knowles MA et al. 2015 and Necchi A et al. 2019.[5][24]
Explore more
Learn more about FGFR alterations and the value of genetic testing:

Footnotes
Figure 1 Legend
APOBEC=apolipoprotein B mRNA editing catalytic polypeptide-like; CD8 T cells=cytotoxic T lymphocytes; CDKN2A=cyclin-dependent kinase inhibitor 2A; E2F3=gene encoding E2F transcription factor 3; EGFR=epidermal growth factor receptor; ELF3=gene encoding E74 like ETS transcription factor 3; ERBB2=gene encoding receptor tyrosine-protein kinase erbB-2; ERCC2=gene encoding XPD protein; FGFR=fibroblast growth factor receptor; KDM6A=gene encoding lysine-specific demethylase 6A; NK cells=natural killer cells; PPARG=peroxisome proliferator-activated receptor gamma; RB1=gene encoding pRB tumour suppressor; STAG2=gene encoding cohesin subunit SA-2; T2=tumour growth into muscle; T3=tumour growth into fat layer; T4=tumour growth outside of the bladder; TMB=tumour mutational burden; TP53=gene encodes p53.
Figure 2 Legend
Cancers included urothelial carcinomas (transitional cell carcinomas) of the bladder, renal pelvis, ureter, and not specified. The majority of aberrations were activating mutations in FGFR3, including S249C (8 instances), R248C (6 instances), Y373C (2 instances), G370C (2 instances), and K650M (1 instance). Three of these FGFR3 mutations are also about to transform cells in vitro (S249C, S248C, Y737C). Frequencies are expressed as percentages of all 126 cases. There were 44 aberrations in 40 cases (4 cases had more than one aberration), so the total is greater than 100%.[23]